In a recent study posted to bioRxiv preprint* server, researchers observed that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) XBB.1.5 monovalent vaccine booster induces robust neutralizing antibodies (nAbs) against emergent variants.
SARS-CoV-2 Omicron XBB sub-variants have reduced the effectiveness of current vaccines, leading to the authorization of monovalent XBB.1.5 vaccines. While preliminary evidence suggests that updated monovalent vaccines boost serum nAb titers against Omicron EG.5.1 and XBB.1.15, their effect on more recent sub-variants (HV.1, HK.3, JN.1, JD.1.1, and BA.2.86) is unknown. The HK.3 sub-variant is responsible for 50% of new infections in Asia. Further, one in every five infections in North America is due to the HV.1 sub-variant. JN.1, JD.1.1, and BA.2.86 sub-variants are spreading in Europe.
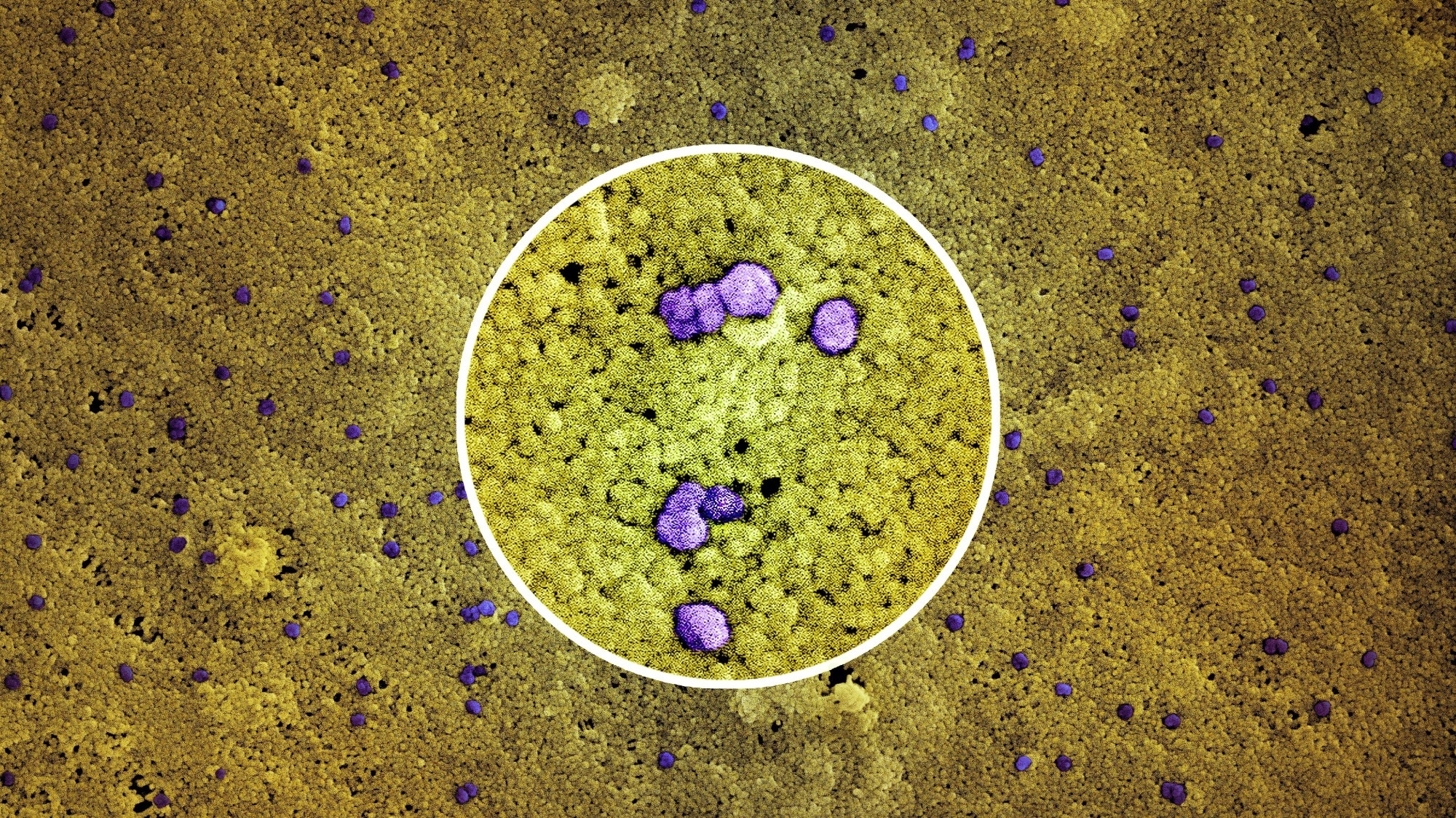 Study: XBB.1.5 monovalent mRNA vaccine booster elicits robust neutralizing antibodies against emerging SARS-CoV-2 variants. Image Credit: NIAID
Study: XBB.1.5 monovalent mRNA vaccine booster elicits robust neutralizing antibodies against emerging SARS-CoV-2 variants. Image Credit: NIAID

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
The study and findings
In the present study, researchers assessed the clinical outcome of monovalent XBB.1.5 mRNA booster vaccination on serum nAbs against the newly emergent Omicron sub-variants. They obtained sera from 60 individuals who were either 1) infection-naïve and boosted with the monovalent XBB.1.5 vaccine (XBB.1.5 MV), 2) XBB-infected but not boosted with the XBB.1.5 vaccine (XBB infx), or 3) Omicron-infected and boosted with the XBB.1.5 vaccine (Omicron infx + XBB.1.5 MV).
All participants received ≥ three doses of the monovalent wild-type mRNA vaccine and one dose of the bivalent BA.5 mRNA vaccine. Boosted individuals with a previous Omicron infection were further stratified into (pre-XBB and XBB infection) subgroups. Individuals in the pre-XBB subgroup were infected before 2023, and those in the XBB subgroup were infected after February 2023.
Pseudoviruses of SARS-CoV-2 JN.1, JD.1.1, HK.3, HV.1, EG.5.1, XBB.1.5, BA.5, and D614G were generated for neutralization assays. After XBB.1.5 vaccination, the XBB.1.5 MV cohort exhibited three- and seven-fold increases in nAb titers against D614G and BA.5, respectively, relative to pre-vaccination. Further, a 13- to 27-fold increase was observed against JN.1, JD.1.1, HV.1, HK.3, EG.5.1, and XBB.1.5 sub-variants.
The XBB infx cohort had a similar neutralization profile post-infection as the XBB.1.5 MV cohort post-vaccination. Notably, the Omicron infx + XBB.1.5 MV cohort produced the highest nAb titers. Nevertheless, this cohort showed smaller increases due to higher pre-vaccination titers induced by the previous Omicron infection.
Furthermore, neutralization after the XBB.1.5 booster vaccination was more pronounced against the newly emergent sub-variants. There were no differences in titers between the two subgroups. The researchers observed that XBB.1.5 infection or vaccination induced the highest neutralizing titers against D614G, followed by BA.5.
The XBB.1.5 sub-variant was more resistant to neutralization than BA.5 and marginally more sensitive than EG.5.1. Titers against the newly emergent sub-variants were similar but lower than against XBB.1.5. The JN.1 sub-variant had the lowest nAb titers. Nevertheless, the absolute neutralizing titers post-XBB.1.5 infection or vaccination were robust against all tested variants.
Further, the team generated antigenic maps using neutralization data. They noted shortened antigenic distances between D614G and other variants after XBB.1.5 vaccination. Moreover, the decrease in antigenic distances post-XBB.1.5 infection was similar to that post-XBB.1.5 vaccination, suggesting that vaccination and infection enhanced antibody responses comparably.
HK.3, JD.1.1, and HV.1 sub-variants formed a cluster and were more distant than EG.5.1 and XBB.1.5. The highest titers after XBB.1.5 vaccination observed for D614G suggested substantial back-boosting of antibodies against predecessor variants, likely due to immunological imprinting. As such, the team compared the severity of imprinting between BA.5 bivalent and XBB.1.5 monovalent vaccinations.
To this end, they extracted data from a previous study on people who received four wild-type monovalent doses and two BA.5 bivalent doses. They found that the second BA.5 bivalent booster elicited similar increases in neutralizing titers against D614G and BA.5. By contrast, XBB.1.5 vaccination or infection-induced much higher increases (> 27-fold) in titers against XBB.1.5 than against D614G (> 3-fold), suggesting less severe immunological imprinting with XBB.1.5 vaccines.
Conclusions
The findings indicate that an XBB.1.5 vaccination or infection markedly elevates neutralizing titers against EG.5.1 and XBB.1.5 sub-variants. nAb titers against the more recent sub-variants increased by 13–27-fold after XBB.1.5 vaccination in infection-naïve individuals and 10-fold in those with a previous Omicron infection. The XBB.1.5 infection notably elicited a neutralization profile similar to the XBB.1.5 vaccination.
Further, the findings highlight that JD.1.1, JN.1, HV.1, and HK.3 sub-variants are more resistant to neutralization than XBB.1.5. Although immunological imprinting was observed with the monovalent XBB.1.5 vaccine, it was not as severe as with the BA.5 bivalent vaccine. Of note, the study did not evaluate mucosal immunity, T-cell responses, or the durability of antibodies.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source link
credite
